2018-01-27 19:36:00金台診所附設醫學美容 Dr.Wu.
Phlyctenular Keratoconjunctivitis
Phlyctenular Keratoconjunctivitis: 12 year-old Female with Staphylococcal Blepharitis
Phlyctenular Keratoconjunctivitis: 12 year-old Female with Staphylococcal Blepharitis
Arpitha Muthialu, MD, Lauren E. Jensen, and Michael Wagoner, MD, PhD
February 27, 2009
Chief Complaint: Blurry vision and discomfort in the right eye (OD).
History of Present Illness: A 12 year-old female complains of blurry vision, foreign body sensation, and photophobia in her right eye. While she has had chronic problems for years in both eyes, she has noted the acute onset and progressive worsening of the symptoms in the right eye for one week.
Past Ocular History: Since the age of 6, the patient has struggled with meibomian gland dysfunction and chronic staphylococcal blepharoconjunctivitis, as well as seasonal allergic conjunctivitis. She has been treated with topical corticosteroids, antibiotics, and antihistamines since age 8 and systemic doxycycline since age 9.
Medical History: Otherwise healthy.
Medications: Since her last exam 8 months prior to this presentation, she was completely asymptomatic on a regimen of:
The patient had discontinued all of these systemic and topical medications one month prior to the current episode upon the suggestion of a maternal aunt who recommended adoption of a "holistic and naturalistic" approach to the managment of her chronic ocular disorders.
- Doxycycline (100mg orally once daily)
- Prednisolone acetate 1.0% (twice daily drops)
- TobraDex (Tobramycin and Dexamethasone) ointment nightly
Family History: Noncontributory
Physical and Ocular Examination:
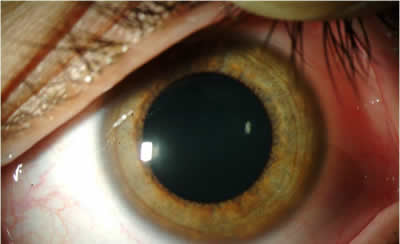
Figure 1A: Right Eye external exam exhibitsFigure 1B: External exam, elevated yellow nodule.
- General: healthy-appearing young female
- Visual Acuity, without correction:
- OD--20/80 (with pinhole improves to 20/50)
- OS--20/20
- Extraocular Motility: Full, both eyes (OU)
- Intra-ocular pressure: OD -- 17mmHg; OS -- 14 mmHg
- External and anterior segment examination (see Figure 1A-C and Figure 2A-B)
- OD
- Lids/adnexa: mild anterior blepharitis
- Conjunctiva/sclera: 2+ diffuse conjunctival injection
- Cornea: 1x1 mm elevated yellow nodule with central erosion and fluorescein uptake with surrounding engorged hyperemic vessels, slightly inferior to the visual axis; there is 360 degree limbal pannus
- Anterior chamber: deep and quiet
- Iris is normal and lens is clear
- OS
- Lids/adnexa: mild anterior blepharitis
- Conjunctiva/sclera: quiet and white
- Cornea: 360 degree limbal pannus
- Anterior chamber: deep and quiet
- Iris is normal and lens is clear
- Dilated fundus exam (DFE): No pallor or edema of either disc. Normal macula, vessels, and periphery, OU
Figure 1C: Anterior Segment ExamMild anterior blepharitis with diffuse conjunctival injection. The cornea shows a 1x1 mm elevated yellow nodule with central erosion and fluorescein uptake with surrounding engorged hyperemic vessels, slightly inferior to the visual axis.
Figure 2A: External Exam. Left eye.Figure 2B: External Exam of left eye shows mild anterior blepharitis
Discussion: Phlyctenular keratoconjunctivitis (PKC) is a localized noninfectious inflammatory/ hypersensitivity disorder of the ocular surface characterized by subepithelial nodules of the conjunctiva and/or cornea. These "phlyctenules," are derived from "phlyctena," the Greek word for "blister." The blister characterization was likely chosen due to the tendency for the nodules to ulcerate once necrosis occurs. Histopathologically, phlyctenules are subepithelial inflammatory nodules containing histiocytes, lymphocytes, plasma cells, and neutrophils. Mononuclear phagocytes, dendrites Langerhans cells, and neutrophils make up the majority of the inflammatory cells in the epithelium overlying the phlyctenule.
The pathogenesis of PKC is thought to be a hypersensitivity reaction to an antigen of bacterial origin. PKC has been classically associated with M. tuberculosis (especially in developing countries). However, Staphylococcus aureus is the cause in majority of cases in the United States. A number of other organisms are also associated with PKC (Table 1).
Table 1: Organisms Implicated in the Pathogenesis of Phlyctenular Keratoconjunctivitis
- Mycobacterium tuberculosis
- Staphylococcus aureus
- Chlamydia trachomatis
- Neisseria gonorrhea
- Coccidiodes immitis
- Bacillus spp.
- Herpes simplex virus
- Leishmaniasis Ascaris lubricoides
- Hymenlepsis nana
- Candida spp.
Most often, phlyctenulosis is a corneal sequelae of chronic Staphylococcal blepharitis, a disorder that often presents in the clinic as chronic conjunctivitis or keratitis characterized by punctate epithelial keratopathy, and/or marginal corneal infiltrates (Table 2). When present, symptoms of PKC depend upon the location of the lesion. Conjunctival lesions usually present with mild to moderate symptoms, including foreign body sensation, tearing, photophobia, burning, and itching. Corneal lesions typically present with more severe symptoms of the same variety.
Corneal phlyctenules usually begin at the limbus and spread centrally, perpendicular to the limbus, leaving no clear zone between the lesion and the limbus. The vessels run in a straight course from the limbus. They can become necrotic and ulcerate centrally or spontaneously involute within 2 to 3 weeks. Upon resolution, a wedge-shaped fibrovascular scar may remain. Centripetal migration of successive inflammatory lesions may develop as in this case. Rarely, inflammation associated can lead to keratolysis and perforation.
Treatment: Management of PKC requires both anti-inflammatory and anti-bacterial management, as well as management of chronic blepharitis. Control of inflammation can be achieved with topical corticosteroids, which should be tapered very slowly to avoid recurrences. Antibacterial measures may include a several week course of application of topical antibiotics to the eyelid margin and conjunctiva, especially at bedtime. Management of chronic blepharitis requires a consistent regimen of lid hygiene and warm compresses, as well as systemic administration of tetracycline derivatives, such as Doxycycline for patients without contraindications. Tetracyclines should not be used in children under age 8 because permanent tooth discoloration can occur. In addition, tetracycline is teratogenic and should be avoided in pregnant women, as well as in nursing mothers.
Follow-up Course: Our patient responded dramatically to topical prednisolone acetate 1% which was initially used every 2 hours while awake. She was treated with a 1 week course of topical gatifloxacin drops four times daily (to prevent infection at the epithelial defect) and a 3 week course of TobraDex® ointment at bedtime. Management of chronic blepharitis was achieved by reinstating a strict program of lid hygiene and warm compresses, along with reinstituting doxycycline 100 mg orally twice daily for one month and then once daily thereafter. Within 1 week, she responded readily to this treatment with improved vision and decreased discomfort (post-treatment images Figure 3A-D), after which topical corticosteroid therapy was gradually tapered.
Figure 3A: Right eye, post-treatmentFigure 3B: Right eye, post-treatmentFigure 3C: post-treatmentFigure 3D: post-treatment anterior eye exam.
Diagnosis: Phlyctenular keratoconjunctivitis
EPIDEMIOLOGY
SIGNS
- Predominantly young individuals
- Staphylococcal blepharitis
- Inflammation of cornea or conjunctiva
- Wedge-shaped nodular lesion and engorged hyperemic vessels at or near the limbus, bulbar conjunctiva, or cornea
SYMPTOMS
TREATMENT
- Redness, foreign body sensation, morning crusting, photophobia, itching
- Decreased vision
- Antibacterial
- Eyelid hygiene
- Ointment to lid margin (i.e. TobraDex)
- Topical antibiotics initially (i.e. gatifloxacin)
- Anti-inflammatory
- Topical corticosteroids (i.e. prednisolone 1% q2-q4 hours)
- Treat the blepharitis
- Eyelid hygiene
- Warm compresses
- Oral doxycycline (100mg Daily to BID)
Differential Diagnoses for Corneal nodule and irritation
References
- Staphylococcal marginal keratitis with phlyctenule
- Microbial keratitis
- Inflamed pseudopterygium
- Salzmann's nodule
- Corneal foreign body
1. Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology. 2nd ed. Philidelphia: Saunders; 2000. p. 1093-1099.
2. Gokhale J et al. Etiology of Phlyctenulosis. Indian Journal of Ophthalmology. 1965. Vol 13 (2): 65-67.
3. Jackson WB. Blepharitis: Current strategies for diagnosis and management. Can J Ophthalmol. 2008 Apr: 43(2):170-9.
4. Krachmer JH, Mannis MJ, Holland EF, eds. Cornea. 2nd ed. Philadelphia: Elsevier Mosby; 2005. p. 1235-1238.
5. Rapuano CJ, Luchs JI, Kim T. Anterior Segment: The Requisites in Ophthalmology. St. Louis: Mosby; 2000. p. 165-168.